Groundswell
Making Space for Grief, Together: Integrated Emotional Support Systems for Oncology Staff
About: Groundswell began as a graduate student project. It has since been awarded a grant for a 12-month pilot program and quality improvement study at UPMC, launching in 2025. The program explores how supporting healthcare workers’ emotional well-being can improve job satisfaction and retention.
Client: UPMC Magee-Womens Hospital
Team: Lorin Anderberg, Elijah Benzon, Kelly McDowell, Robertus Shuyo
Course: Designing With CARE for Oncology: Co-Creating Solutions to Complex Care Coordination—Carnegie Mellon University
Credits: Professor Kristin Hughes, Dr. Sarah Taylor, Dr. Grace Campbell, AI Imagery
Duration: 15 weeks—Ongoing
Press: CMU Article
Design Challenge:
Create supportive environments where staff can feel nurtured, recognized, and celebrated.
How might we create supportive environments tailored for the well-being of healthcare staff, enabling them to openly and safely discuss and express concerns such as burn-out, compassion fatigue, the emotional toll of patient deaths, and the increasing frustration arising from administrative tasks overshadowing patient care?
Process:
Research
3 Weeks
Internet Research
Hospital Shadowing
User Interviews
Research
3 Weeks
Participatory Event
Participatory Workshop
Affinity Mapping
Ideation
3 Weeks
Brand Identity + Concept
Mid-Point Presentation
Revisions
Feedback
3 Weeks
Speed Dating
Revisions
Stakeholder Crit
Presentation
3 Weeks
Client Presentation
Feedback
Grant Approval!
Launch
8 Weeks
Brand Refinement
Production
Training
Concept:
15-Week Course:
Through trust building, observational and generative research, rapid ideation, and feedback sessions our team developed the first iteration of the Groundswell concept and pitched it to the staff at UPMC hospital in May 2025. We were able to get 2 NookPods donated (a $30k value).
We learned about the phenomenon of “chronic compounded grief” among oncology nurses, and how repeated exposure to loss accumulates over time when not properly processed. We want to help build a future where your wellbeing is the centerpiece of the healthcare system. Listen to the poem we wrote, it was inspired by what we heard in our interviews:
Pilot Study Launch:
Post grant approval, a subset of the team stayed on to bring the initial Groundswell concept into a production for the 12-month study. Through more feedback sessions with UPMC we revised the core concept, updated the brand, changed the visual style, got admin approval and collaborated on the quality improvement research assessments.
(In progress, preview available upon request)
Ecosystem:
The final design proposal that we presented to University of Pittsburgh Magee-Womens Hospital Gynocologic Oncology Staff.
Groundswell, Making space for grief, together.
Named for water rising naturally from within the earth, Groundswell is designed to support the emotional well-being of staff at UPMC Magee-Womens Cancer Services. Through communication, creativity, and connection, Groundswell fosters a culture where the emotional complexities of oncology care are acknowledged, isolation transforms into belonging, and self-care is honored as essential to delivering excellent patient care.
Core Components:
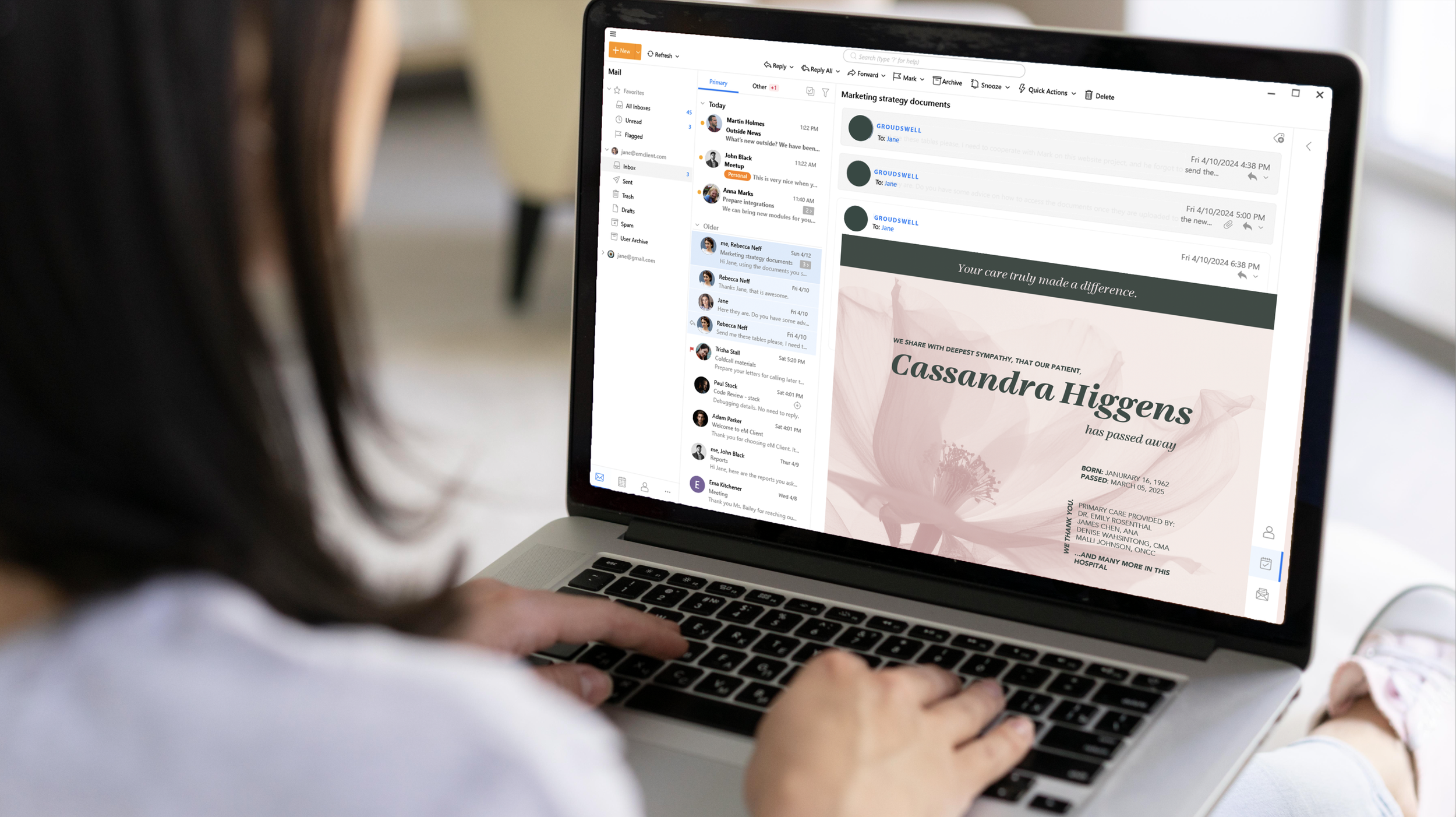
Updated patient death notification email template with compassionate visuals and language that acknowledges the impact of patient loss
A restorative pod space for emotional decompression and restoration through research-backed mindfulness activities
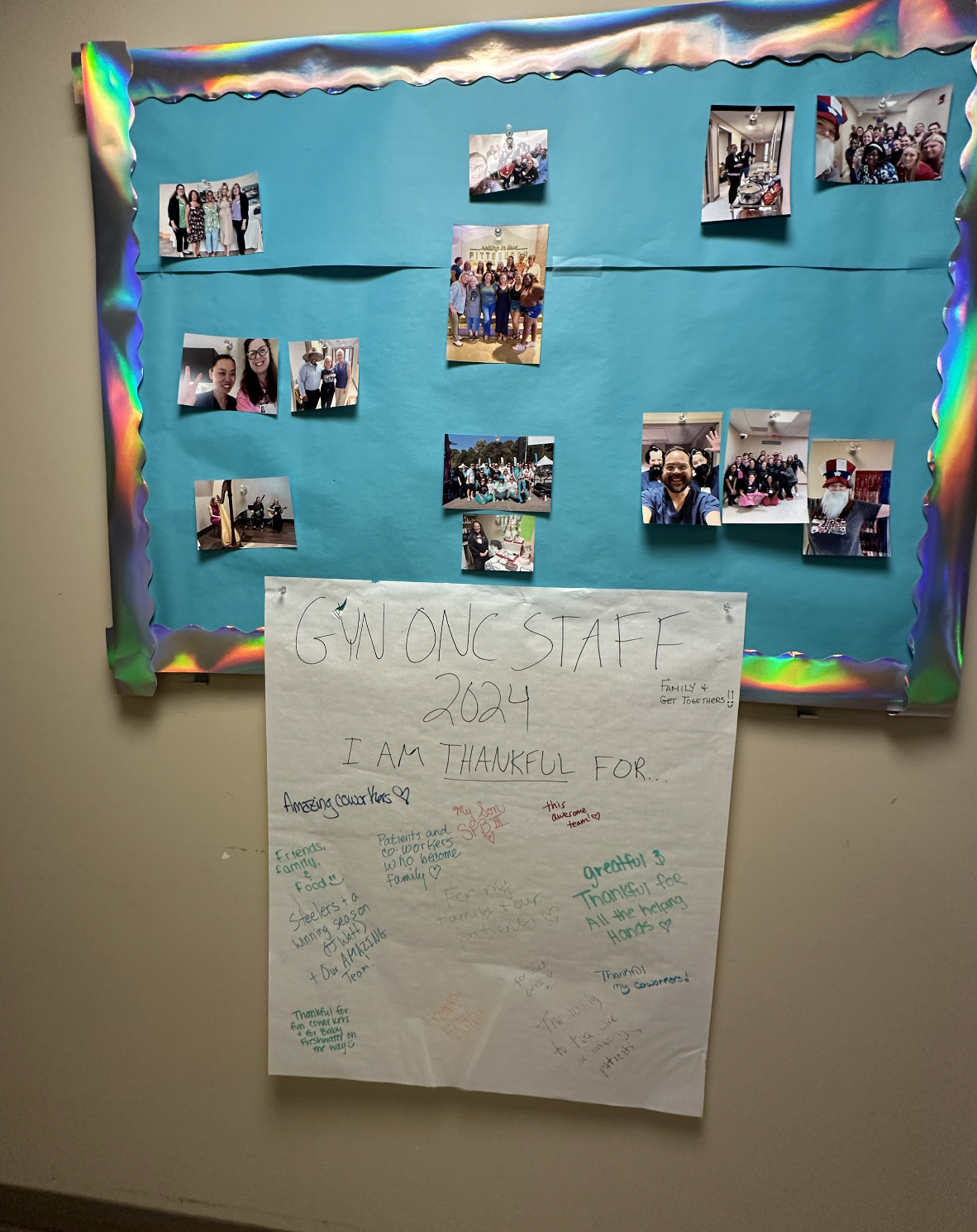
A community art wall that invites participation through shared emotional expression about the emotional complexities of oncology care
A training guide on how to speak about grief and make space for vulnerable conversations in the workplace
We shadowed at Magee, interviewed 8 employees, and conducted 2 generative research workshops.
We learned that many of the staff at Magee save their tears and emotional outlets for the car ride home or the bathroom stall—a process that takes away from their quality time with loved ones.
Almost every person we spoke to commented on the physical office environment as a strong opportunity for improvement.
We heard in our interviews that most staff have a hard time talking about the emotional complexities of their work with friends and family because they may not fully understand.
And that staff either are not aware of resources available to them or do not feel those resources are sufficient/accessible.
We also heard that some may not feel comfortable speaking up about what is weighing on them.
Research shows that art therapy interventions have proven effective in addressing healthcare worker burnout (a failure of institutional support of employee well-being not the failure of an individual) and we know from our research that staff at Magee perceive value in creative expression in the workplace.
This informed our idea to create an outlet for staff to express themselves freely without consequence while also cultivating a sense of belonging to the greater community:
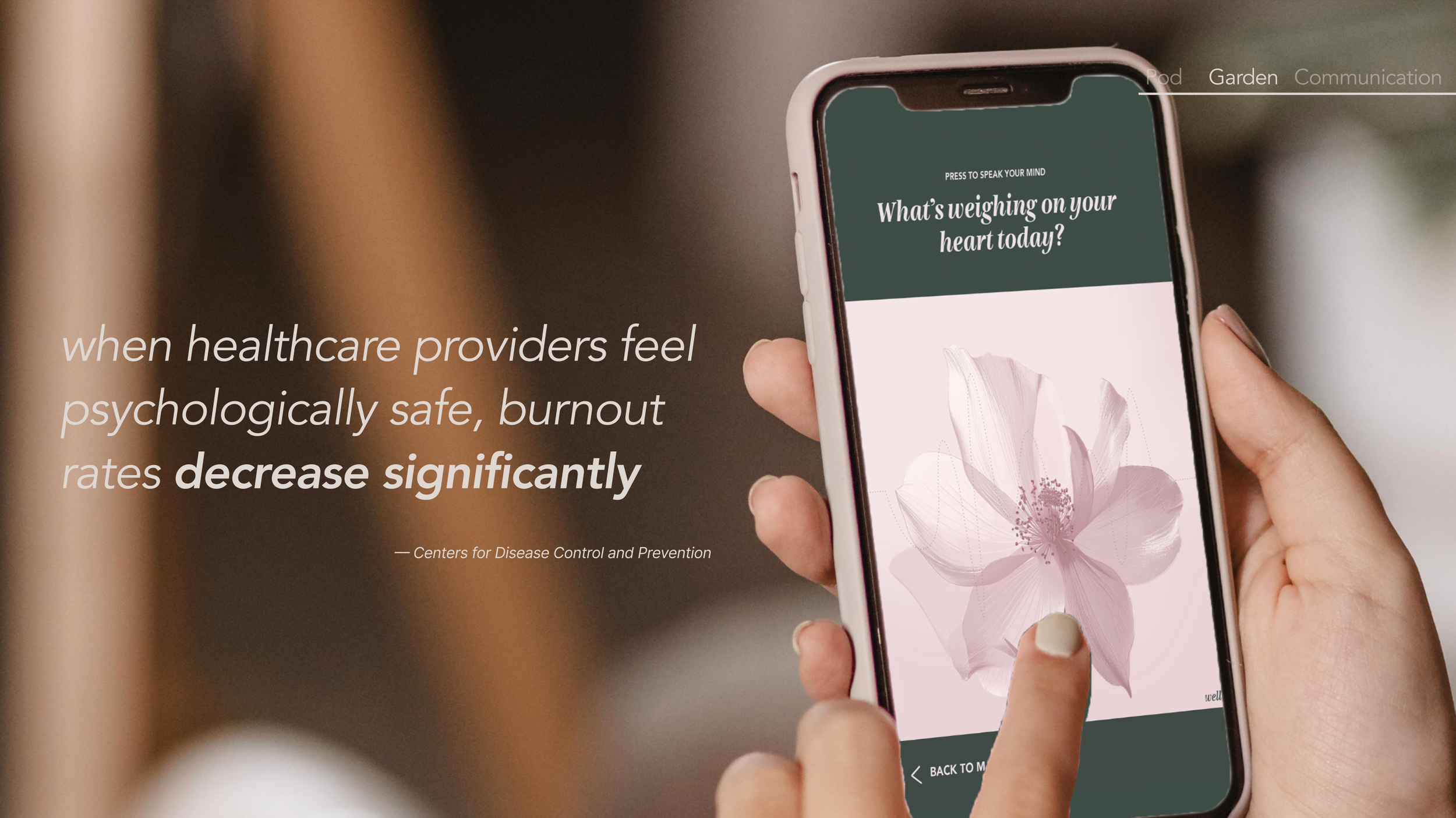
The groundswell garden: A digital platform where staff anonymously voice emotions that transform into flowers within a collective visual display.
Staff simply speak their thoughts into the app, and instantly, a unique digital flower blooms on our display. As these expressions accumulate, similar emotions cluster together, growing larger when many share the same experience.
Behind the scenes, our system recognizes these patterns, giving leadership valuable anonymous insights without anyone having to speak up individually. The Garden helps staff externalize grief rather than carrying it home.
The anonymity of the Garden is critical—research shows that stigma often prevents healthcare workers from expressing their emotions openly.
While tangible solutions are important, it’s often the smallest adjustments in how we communicate that ripple outward to create the most profound cultural change.
This brings us to the final element of our ecosystem: the groundswell communication guide. We propose a new approach to discussing the emotional aspects of oncology work—one that invites participation, acknowledges complexity, and validates lived experience.
And studies show that acknowledging healthcare workers’ emotional labor is essential to preventing burnout. Research demonstrates that subtle adjustments to language and mindful communication can create measurable cultural change.
We propose a new approach to discussing the emotional aspects of oncology work in a way that invites participation, acknowledges complexity, and validates the experiences of healthcare workers.
The groundswell communication guide serves as a comprehensive training for the Groundswell Champion who will steward the program—teaching them how to lead with authenticity while creating supportive spaces for honest feedback, shared vulnerability, and community celebration.
These training materials transfer effectively between champions, ensuring that Groundswell evolves from a pilot initiative to sustained movement. This communication guide shifts our language from patient-centered clinical terminology to care worker-centered empathy.
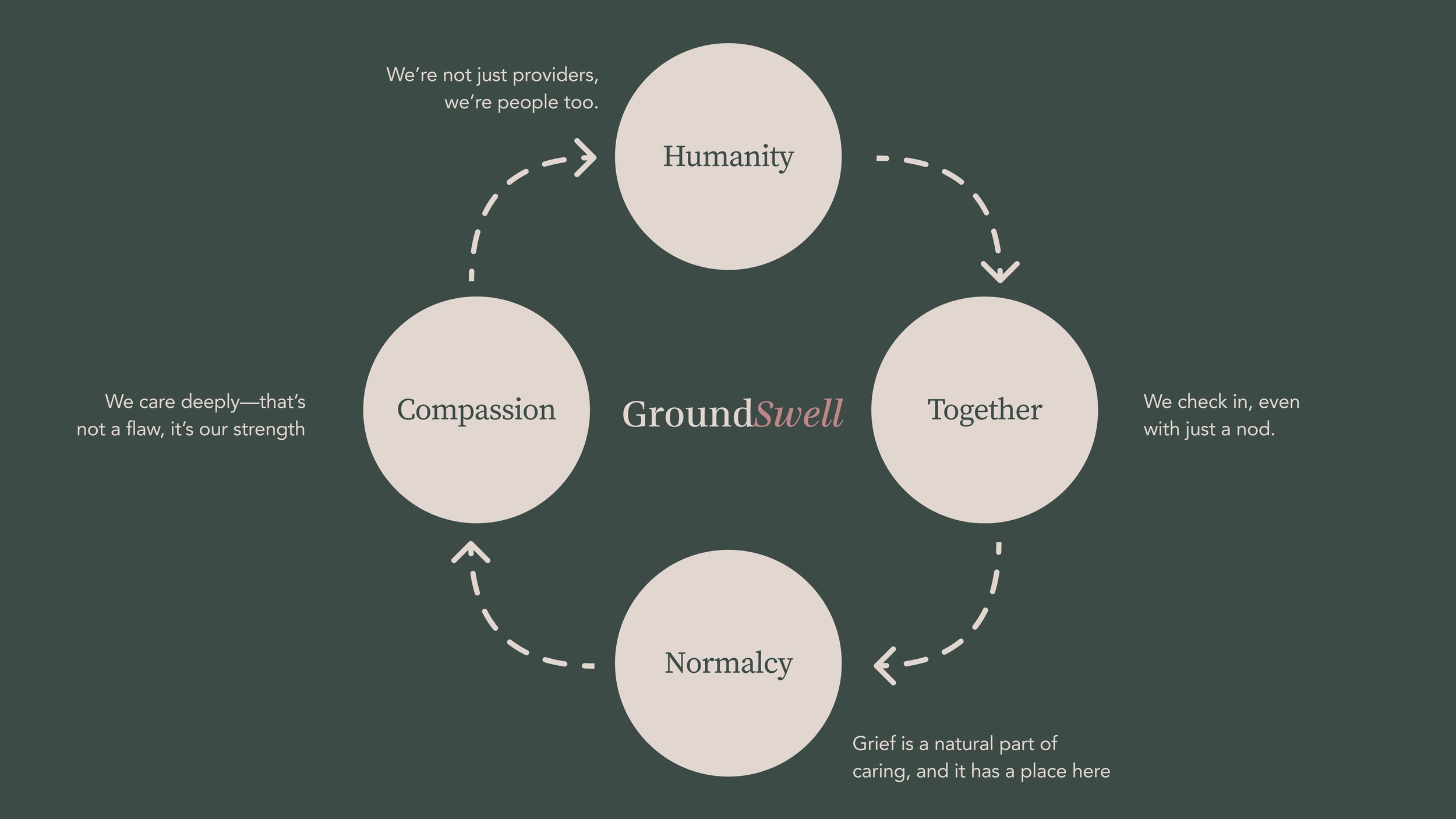
New employees encounter Groundswell’s foundational values, compassion, humanity, togetherness, and normalcy, during onboarding through a flower folding activity.
The symbolic flower they create becomes more than a desk decoration; it serves as a daily reminder that support is available.
While this guide encompasses many aspects of workplace communication, it begins with one simple, immediate change—transforming the standard patient death notification, currently referred to as the Ceased to Breathe email.
By naming not just the patient who has died but everyone who cared for them, we create a moment of collective acknowledgment—We validate their contribution and create space for their grief.
This powerful first step requires no budget, no additional staffing, and no complex training—just a simple Outlook email template that can be implemented tomorrow.
This isn’t merely about changing an email. It’s about declaring that grief deserves space in our professional lives. That noticing someone’s emotional labor is as important as tracking their clinical outcomes. That what remains unspoken eventually becomes unbearable.
This single shift creates the conditions for everything else to emerge. The most profound revolutions begin with the simplest acts. Change how you speak about grief today, and you change how your team experiences it tomorrow.
We come together like water through soil, a groundswell of quiet strength gathering force.
For what you carry, we carry.
Preliminary
Research:
Understanding the Landscape
Internet Research
Stakeholder Analysis
Project goals
Tools
Google Docs
Key Research Findings:
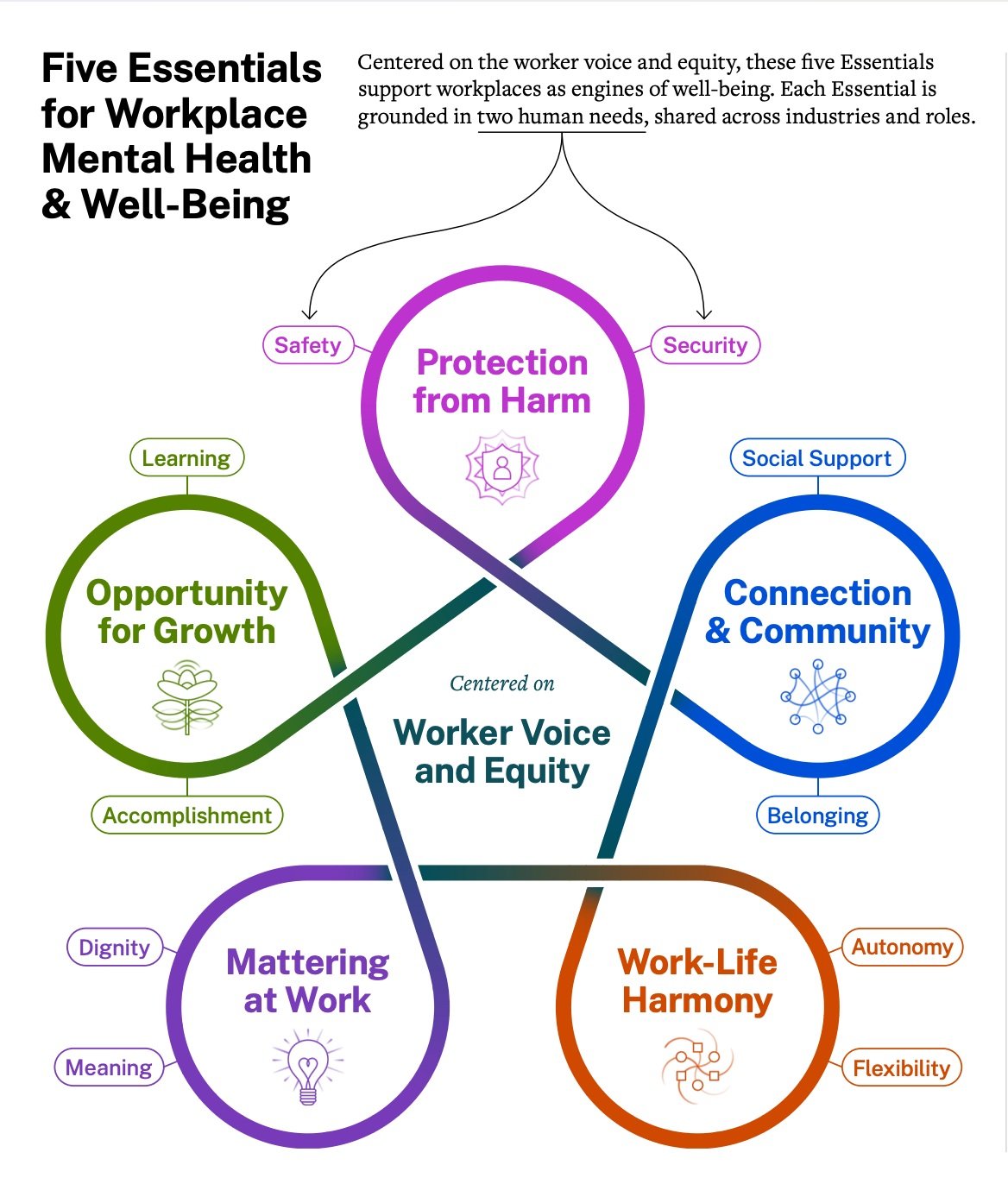
76% of U.S. workers have experienced at least one symptom of a mental health condition
87% report that their work conditions have caused mental health challenges (U.S. Surgeon General, 2022)
Oncology nurses experience "chronic compounded grief" where repeated exposure to loss accumulates over time when not properly processed
Positive workplace conditions are directly associated with less burnout and better mental health (CDC, 2022)
Open and honest communication in healthcare settings leads to higher perceptions of support and lower stress and burnout (National Library of Medicine)
Design Challenges:
Mental health challenges in the workplace, particularly within healthcare settings, are a genuine concern.
Mental health challenges in healthcare settings often stem from the inherently “caring” nature of the work combined with the burden of excessive administrative and clerical tasks.
Addressing mental health issues in the workplace can be achieved through both top-down and peer-to-peer approaches
The stigma surrounding mental health issues has hindered the acceptance and adoption of mental health care.
“The capacity to remain clear about the ‘self-other’ distinction is called emotion regulation. Without emotion regulation skills, our ‘self-other’ distinction is blurred so we absorb another’s suffering and negative emotions as our own and experience empathic distress fatigue. Yet, much of this knowledge is not implemented within the nursing context…healthcare leaders cannot address the distress of its workforce and strengthen cultures without understanding its causes.” —Science Direct
Conclusions:
1. The Dual Burden of Care Healthcare workers face emotional exhaustion from both the inherently compassionate nature of their work (constant exposure to grief, loss, and trauma) and excessive administrative tasks that disconnect them from their original purpose of patient care.
2. Stigma Prevents Help-Seeking 73% of emergency physicians report stigma around mental health treatment in their workplace, with 27% avoiding treatment entirely due to fear of professional consequences—highlighting the urgent need to normalize emotional support in healthcare settings.
3. Support Requires Both Top-Down and Peer-to-Peer Approaches Effective mental health support combines organizational leadership initiatives (psychoeducation, transparent policies) with peer recognition programs, creating a comprehensive culture that prioritizes staff well-being alongside patient care.
Project Timeline:
Key Considerations & Assumptions:
Emotional & Mental Well-being: Clinicians often feel isolated in their grief and burdened by workplace hierarchy.
Environmental Challenges: Stale workspaces, poor lighting, and lack of visual inspiration contribute to burnout.
Recognition & Support: A system for acknowledging good work and offering space for reflection could improve morale.
Administrative Barriers: Excessive paperwork and unclear navigation interfere with patient care.
Design Objectives:
Can Be Implemented Tomorrow: Our solution should be intuitive, requiring minimal training or disruption.
Has Immediate Impact: It should provide clear, tangible benefits, addressing clinician challenges at critical moments.
Respects Existing Structures: We won’t reinvent the wheel or assume we know better than the staff already working in this space.
Doesn’t Overcompensate: We address clinician needs at the time of patient death, not broader issues like scheduling inefficiencies.
Serves Urgent Needs: Our objectives will evolve as we synthesize data, refining our approach to stay aligned with real needs.
Does Not Burden: We will not impose unnecessary complexity
Generative
Research:
Understanding the Problem
On-site User Shadowing
AEIOU
15-Minute Interviews (5)
45 Minute Interview (1)
Women in White Coats Event Participatory Activity
Grief Participatory Activity
Tools
Figma
Google Docs
Medium
Canva
Women in White Coats Participatory Research:
Our team was invited to attend CancerBridge’s Women in White Coats dinner event as an opportunity to do some generative research on our topic. We came up with the idea to create a participatory activity that would allow us to both collect answers in the moment as well as introduce attendees to a targeted survey that would help us better understand compassion fatigue and self care.
A poster of an orchid with a stem featuring our design research question of the night featuring pink orchids are often the flower of choice for breast cancer awareness.
“How has your approach to patient care evolved over time to help you balance compassion and self-care?”
Postcards that expressed a heartfelt thank you message for the important work these women do with an invitation to participate in an online survey via a QR code.
A survey on Google Forms that asked targeted questions for an audience of doctors featuring 5 questions with diverse formats to keep engagement and language targeted at this audience of mostly leaders and doctors.
Generative Research Workshops:
The research team conducted two complementary workshops at Magee to gather different perspectives from staff: the "Nourishing Flower Workshop" (5-15 minutes) focused on quantitative data about broad workplace issues, while the "Grief Workshop" (30 minutes) provided in-depth conversations specifically about grief and coping mechanisms among healthcare practitioners. After testing an initial "hero" workshop that proved too long and disconnected, the team split their approach to capture both breadth and depth of information while ensuring participants felt the experience was genuine and worthwhile for their time investment.
Key Research Findings
The research revealed that healthcare workers at Magee are eager for dedicated spaces to process grief, with participants requesting more time for such discussions and showing that grief management varies widely—some compartmentalize during commutes while others prefer talking through emotions with trusted colleagues. Through the "Nourishing the Flower" workshop, staff across departments emphasized the critical importance of recognition (feeling appreciated through verbal affirmations and acknowledgment), supportive environments (flexible workplaces with adequate resources and comfortable spaces), and strong team culture (collaboration, shared purpose, and kindness) for thriving at work.
Common Challenges and Solutions
The biggest frustrations centered on lack of recognition despite hard work, inadequate resources including insufficient space for both work and decompression, and toxic workplace dynamics that create burnout and affect patient care. Simple, actionable solutions emerged from the research: more verbal affirmations, designated spaces for grieving or relaxation activities like coloring, access to snacks and comfortable break areas, improved communication around patient deaths, and more peer discussions on grief—all of which could significantly impact morale and well-being without requiring major budget increases or external resources.
What we would do differently:
The ‘Nourishing the Flower’ activity was a success, but we do wish we had more time to test it beforehand. An earlier trial would have given us a better sense of how the audience might engage with it and allowed us to make any necessary adjustments to improve the experience.
Excerpt from Facilitation Script
“Part of this exercise is acknowledging and realizing that there is no one size fits all framework for grief. We believe that this workshop will help uncover hidden truths and help start to facilitate these tough conversations and normalize them in the workplace.
We interviewed the staff here at Magee and came to understand that the constant and immense grief of working in oncology can feel impossible to hold, and for some, it may feel easier or safer to numb yourself in order to protect yourself from really feeling the weight of it.
You all are in this work for a reason, because you have an enormous heart and immeasurable dedication to improving people’s lives during the worst moments. You are their cheerleader but so often no one is there to be a cheerleader for you and the workload keeps you just busy enough to get by but with no outlet for your feelings. This is one of the major contributing factors to burnout and empathy fatigue.
If it feels safe and comfortable to you, we invite you to put your hand on your heart and close your eyes, drop into your body and take a deep breath, maybe a few deep breaths so we can center in on identifying what it might look like to receive the kind of support and nurturing that you need during your hardest moments at work.
Let’s take 3 minutes to breathe and be softly thinking about what you might need to hear, receive, or have taken off your plate to feel relief when the grief feels like too much to hold alone. Or just take a moment for you to relax and rest.”
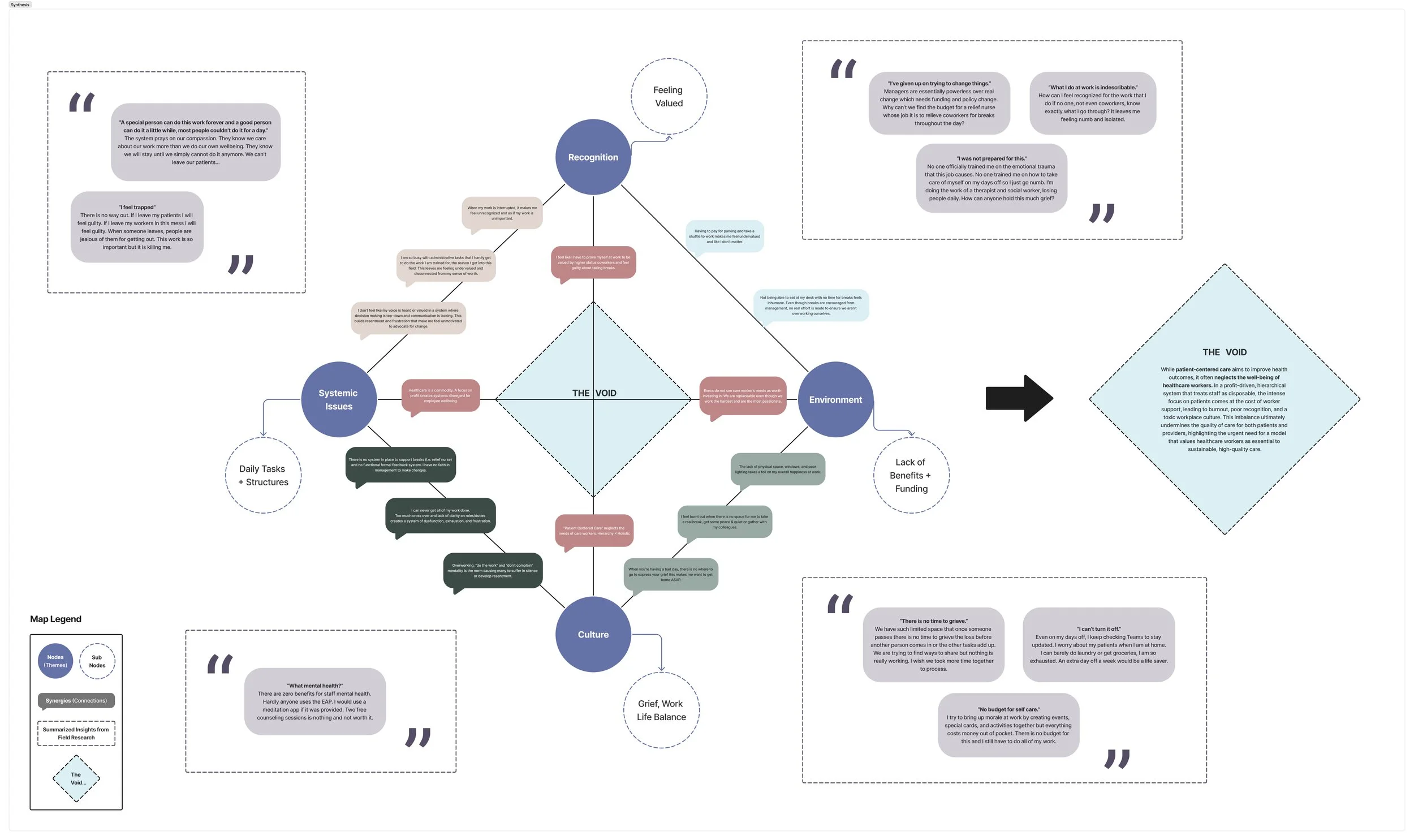
Synthesis:
Understand: Identifying the Root
Affinity Mapping
Tetrahedron Problem Analysis
Tools
Figma
Google Docs
Medium
The research findings support the hypothesis that patient-centered healthcare systems neglect worker well-being, revealing systemic issues including disconnects between staff and leadership due to poor feedback systems, power dynamics between roles, generational tensions, and inadequate physical environments that contribute to burnout.
Healthcare workers face daily challenges from insufficient funding, lack of benefits, overwhelming tasks, poor recognition, limited breaks, and particularly unaddressed grief culture in oncology work where emotional toll remains a "silent burden" without proper processing spaces.
Current solutions like informal recognition efforts (Snap Jar), minimal grief support (obituary walls), and basic wellness amenities (free coffee) are underfunded and treat staff well-being as an afterthought rather than institutional priority, highlighting the urgent need for systematic changes including structured communication channels, funded recognition programs, designated grief processing spaces, improved physical environments, and cultural shifts that genuinely prioritize healthcare worker sustainability alongside patient care.
We took our notes from shadowing and organized them on the board searching for emerging patterns and themes. We then associated perceived emotions that would be felt by healthcare workers as a result of the key themes. We sorted our major issue areas onto a tetrahedron diagram to search for synergies and relationships between different aspects of the problem space. Here, we used theoretical “I” statements to embody the experiences we observed and formulated quotes that represent a summation of what we heard and witnessed.
Ideation:
Imagining a Better Future
Crazy 8 rapid ideation
Peter Pan
Speed dating feedback
Tools
Figma
Google Docs
Medium
Design Principles:
Keeping Mental Well-Being at the Center
Any proposed intervention should prioritize emotional and psychological support for healthcare workers, addressing both systemic issues (workload, leadership support) and peer-to-peer connections (recognition, safe spaces).Balancing Administrative and Caregiving Tasks
We should focus on solutions that alleviate unnecessary clerical burdens, allowing staff to reconnect with patient care and their original motivations for entering the field.Addressing Stigma and Accessibility
Mental health resources must be easily accessible and de-stigmatized, ensuring staff feel safe seeking help without fear of professional repercussions.Using a Holistic, Research-Backed Approach
Our methodology should continue to incorporate firsthand insights (shadowing, interviews) and established best practices (leadership training, peer support systems) to create meaningful, evidence-based interventions.
Feedback:
Feedback from multiple stakeholders revealed key insights and suggestions for refining the healthcare worker well-being solutions, including the need to diversify research beyond just women participants, address practical implementation questions around parking passes and survey management, and rename "compassion fatigue" to "empathy fatigue" based on emerging neuroscience research.
Stakeholders appreciated the research approach and solutions, particularly the ROI calculator and flower workshop, while suggesting integration strategies such as using parking passes as incentives, incorporating biophilic design principles, varying workshop topics to maintain engagement, and considering high turnover rates in healthcare. The team concluded that their solutions could work synergistically as an integrated staff well-being program combining recurring wellness events, data collection for the ROI calculator, a point-based reward system with parking pass incentives, and card games to facilitate meaningful conversations, while being mindful of Goodhart's Law to prevent metric manipulation in the ROI calculator design.
Iteration:
Brand Feel
Earthy
Calming
Supportive
Authentic
Launch:
Grant Funding
Groundswell was awarded a UPMC grant to pursue the installation of our proposed project for a 12-month quality improvement research study that will measure employee well-being, team cohesion, and intent to leave before, during, and after the installation. The project components have evolved and the brand has shifted through iterative co-design and feedback from stakeholders. We have received over $30k worth of donations for material and production skills to make this project a reality and are hopeful that this study will prepare us for the next iteration in more hospital settings.
Principal Investigators:
Kristin Hughes, MFA, Professor, CMU
Sarah E. Taylor, MD, PhD, UPMC Hillman Cancer Center
Supervising Faculty:
Grace Campbell, PhD, RN, Family CARE Center
Heidi Donovan, PhD, RN, University of Pittsburgh School of Nursing
A Research-Based Pilot Program Supporting Healthcare Workers in Oncology
The Hidden Crisis
Oncology staff in hospitals across the United States face a cyclical emotional burden that remains largely unacknowledged by healthcare systems. The daily experience of holding space for suffering, delivering difficult news, and witnessing death takes a significant toll on healthcare workers’ emotional well-being, increasing the risk of compassion fatigue and burnout¹.
The Research Foundation
This work emerged from "Designing with CARE: Co-Creating Solutions for Complex Care Coordination in Oncology," a graduate-level design course taught by Professor Kristin Hughes in partnership with UPMC Magee-Womens Hospital. Through extensive fieldwork, interviews, and shadowing experiences, the research team identified that staff at Magee-Womens Cancer Services experience significant emotional strain, including what research terms 'chronic compounded grief.'² Studies show that grief, sense of failure, and exposure to suffering are key contributors to compassion fatigue among oncologists¹.
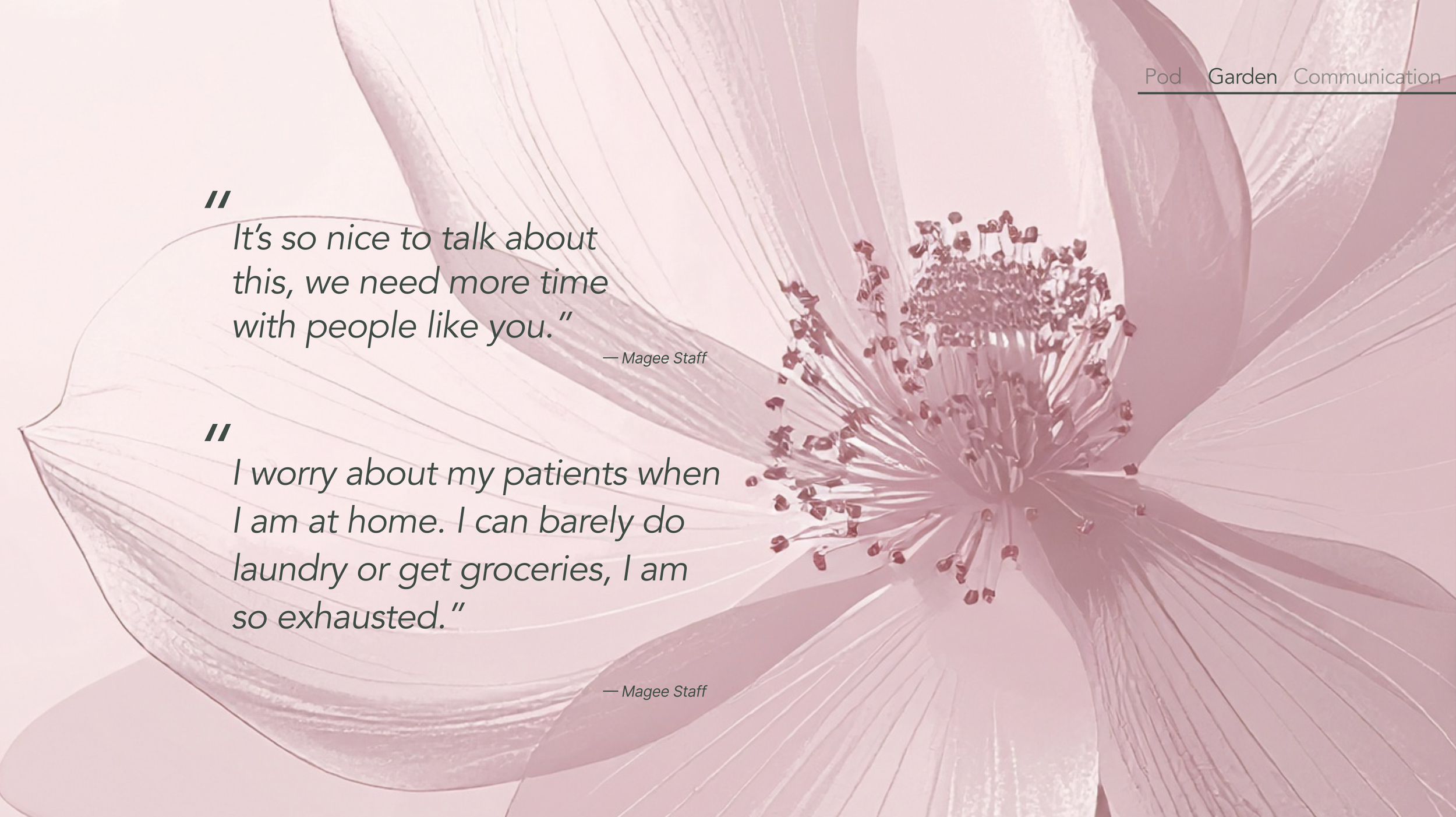
In preliminary research interviews, staff mentioned:
"No one trained me on how to take care of myself on my days off, so I just go numb."
"I worry about my patients when I am at home. I can barely do laundry or get groceries, I am so exhausted."
The Solution: Groundswell
Groundswell is a 12-month pilot program designed to support the emotional well-being of UPMC Magee-Womens Cancer Services staff by introducing resources that honor the emotional complexities of oncology care. Inspired by the existing network of support among staff and named for water that rises naturally from deep within the earth, this comprehensive initiative recognizes that the most meaningful support emerges from within the care community itself. Through communication, creativity, and connection, Groundswell fosters a culture where grief is acknowledged, isolation transforms into belonging, and self-care is honored as essential to delivering excellent patient care.
The program creates a supportive ecosystem that emerges from within the care team itself, addressing a critical gap in healthcare: the need for structured emotional processing interventions in high-mortality settings¹.
Core Components:
Updated patient death notification email template with compassionate visuals and language that acknowledges the impact of patient loss
Restorative pod space for emotional decompression and restoration through research-backed mindfulness activities
Community art wall that invites participation through shared emotional expression about the full spectrum of experiences in oncology
Guided reflection cards that help staff build a self-care practice through emotional validation and introductory exercises for nervous system regulation
Why This Matters Now
In a healthcare system facing unprecedented staffing challenges, this research addresses workforce sustainability at its core. As one Magee nurse shared:
"A special person can do this work forever, a good person can do it for a little while, most people couldn't do it for a day."
Rather than relying on exceptional individuals to shoulder impossible burdens, Groundswell creates systemic solutions that make compassionate care sustainable for all healthcare workers.
Pilot Objectives
Objective 1: Assess the feasibility and acceptability of integrating the Groundswell communication framework into the Magee Gynecologic Oncology Program.
Objective 2: Evaluate the impact of structured, grief-acknowledging communication processes on clinic provider and staff self-reported compassion fatigue scores, emotional exhaustion, chronic compounded grief, and intention to leave within the next 6 months.
Objective 3: Examine the role of a dedicated grief processing space (Groundswell Pod) in staff perceptions of emotional labor legitimacy, ability to maintain appropriate emotional boundaries, and team cohesion and support behaviors.
Objective 4: Develop and prototype a peer-support platform that fosters emotional expression, connection, and community cohesion among staff.
Expected Outcomes
This pilot will deliver a structured support intervention that helps staff create space to acknowledge and process the profound human experiences inherent in oncology work. With integrated systems designed to restore emotional well-being, Groundswell aims to reduce burnout, compounded grief, and turnover intentions—creating evidence-based solutions that can be implemented in standard practice across healthcare settings.
This approach represents transformative potential for workforce sustainability by moving beyond individual resilience to create regenerative systems of support. By honoring the emotional labor of healthcare workers and providing pathways for restoration, Groundswell recognizes that supporting those who dedicate their lives to caring for others is not just compassionate—it is essential to providing exceptional patient care.
Project Production Team:
Kristin Hughes, MFA, Professor, Carnegie Mellon University
Lorin Anderberg, MA in Design, Carnegie Mellon University
Elijah Benzon, MA in Design, Carnegie Mellon University
Greg Baltus, Fabricator/Builder Industrial Design
Project Development Team:
Lorin Anderberg, MA in Design, Carnegie Mellon University
Elijah Benzon, MA in Design, Carnegie Mellon University
Kelly McDowell, Art and Design, Carnegie Mellon University
Robertus Sucahyo, MBA, Carnegie Mellon University
References:
¹ Laor-Maayany R, Goldzweig G, Hasson-Ohayon I, Braun M, Galinsky D, Baider L. Compassion fatigue among oncologists: the role of grief, sense of failure, and exposure to suffering and death. Support Care Cancer. 2020 May;28(5):2025-2031. doi: 10.1007/s00520-019-05009-3.
² Feldstein MA, Gemma PB. Oncology nurses and chronic compounded grief. Cancer Nurs. 1995 Jun;18(3):228-36.
*Groundswell acknowledges that the term burnout is a reflection of institutions’ inability to support staff well-being and not an individual failure.